No products in the cart.
Explore
Contact Us.
We're ready to help.
Looking for more information, or to be connected with your local representative?
We can help. Fill out our contact form to get started.

24
May
Who is the Best Candidate for an Innovative Lymphatic Surgery?
This is an 11-minute read.
For me, as a lymphedema reconstructive plastic surgeon, everything is centered around patient care and looking at things from the patient’s point of view. Each patient has a unique journey when it comes to discovering and treating their health condition.
It’s important to start from a place of compassion and keep in mind that someone with a chronic disease may be facing a life-changing operation. Patients need help understanding how lymphatic surgery works and whether they’re truly a good fit for it.
In this article, I’ll discuss who’s an ideal candidate for reconstructive plastic surgery from a lymphedema surgeon’s point of view.
Choosing the Right Surgery for the Right Patient
Everything begins with a thorough understanding of the patient’s condition and choosing the appropriate surgery(s) for the patient. I have created an integrated lymphedema treatment system, the Granzow SystemSM, which encompasses surgical and non-surgical treatments. Each patient is prescribed their unique treatment plan.
These three types of surgeries are part of:
- Vascularized Lymph Node Transfer (VLNT Surgery)
- Lymphaticovenous Anastomosis (LVA Surgery)
- Suction Assisted Protein Lipectomy (Granzow SAPLSM Surgery)
A patient must first undergo a thorough clinical evaluation by our team. Our treatment recommendations include surgery, lymphedema therapy, and other options for before and after surgery to optimize long-term success.
For a patient with stage 1 lymphedema in the right arm, I may prescribe microsurgeries that can reconstruct the lymphatic system such as VLNT or LVA surgeries. VLNT surgery involves moving lymph nodes and a small amount of surrounding tissue from one part of the body to the other safely and effectively. LVA surgery directly connects the lymphatic system to the venous system for a significant improvement in lymphatic fluid drainage.
The Granzow SystemSM – The World’s First Integrated Lymphedema Treatment Program
I developed the first comprehensive lymphedema treatment system that integrates lymphedema therapy and lymphedema surgeries that address both the solid and fluid swelling caused by lymphedema. This treatment system provides proven safe and effective results for patients.
The System’s primary focus is on patient care. Proper patient selection for each surgery is critical and proper aftercare is essential to the ongoing success of the procedures. In addition, all patients will have better post-surgical outcomes with proper lymphedema therapy administered by a certified lymphedema therapist. Using this System, we can consistently achieve long-term improvements in our patients’ quality of life, especially in preventing cellulitis infections.
The Benefits of Lymphedema Surgery
Our studies have shown that our patients experience reductions in arm or leg volume excess average 86% to 111% within one year after surgery. A volume excess reduction of over 100% means the volume of the affected. In most cases, our patients can reduce their reliance on compression garments. You can read more about these results on our website.
Fluid vs. Solid-Predominant Lymphedema
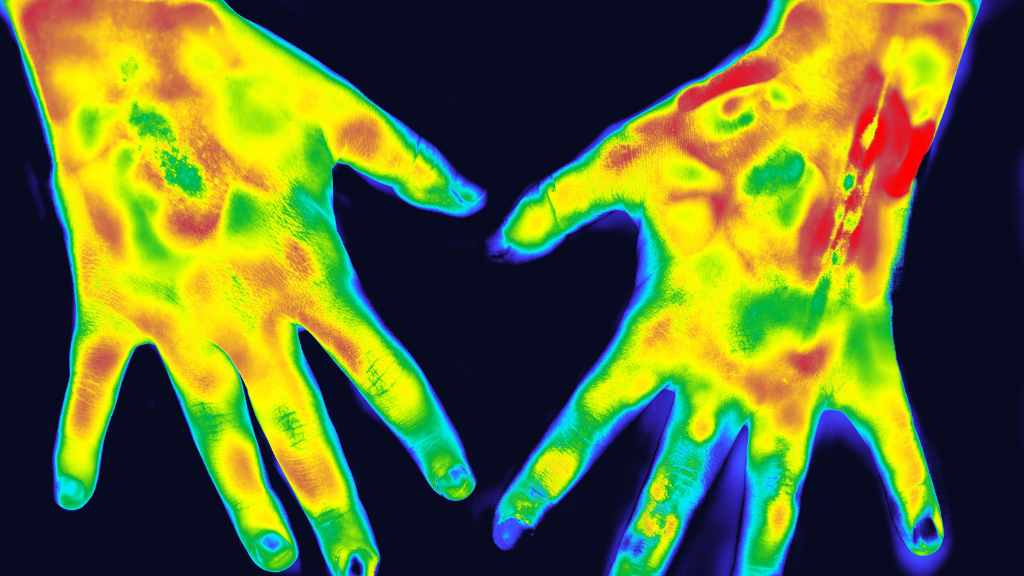
Now let’s look at the difference between fluid predominant lymphedema and solid predominant lymphedema. The distinction is quite important in terms of deciding where a patient is in the disease process and whether a patient is a candidate for which type of surgical procedure.
The lymphatic system is part of the immune system and involves the circulation of lymphatic fluid called lymph. If this circulation is impaired, perhaps through cancer treatment or a congenital cause, the fluid doesn’t drain properly and there is a backup that causes swelling. This is fluid-predominant stage 1 lymphedema. An analogy would be that the patient has a small stream inside that is blocked by a dam building up a lake full of fluid.
This fluid is toxic. It causes damage to the surrounding tissues and further damages the remaining lymphatic system, which in turn worsens the drainage and causes more inflammation. Additional fluid builds up, then the cycle continues.
Eventually, permanent solids develop and deposits, which are fat and proteins, begin to appear. These deposits can’t be removed simply by addressing the fluid. This stage in the lymphedema disease process is called stage 2, solid predominant lymphedema and is a turning point because it impacts the treatments we can provide.
Treatments for the fluid form of lymphedema include microsurgical procedures such as LVA and VLNT, which can drain the fluid but can’t remove solids. When a patient is already in stage 2, solid predominant lymphedema, microsurgery can’t effectively reduce the size of their arm or leg because it cannot remove these solids.
First-line therapy is always conservative lymphedema therapy. It helps prevent the disease from progressing and decreases the excess fluid present. Conservative therapy also helps differentiate who needs surgery and who doesn’t. For example, consider a patient who has lymphedema secondary to having morbid obesity. This patient may not need Granzow SAPLSM surgery to remove solids. Removal of excess fluid alone may improve their condition tremendously.
Lymphatic Surgery Patients and Their Results
Granzow SAPLSM Surgery Patient 1:
This is a patient with breast cancer and chronic stage 2 lymphedema for 19 years. The patient has what most therapists would think of as a very hard case to treat. She has had repeated attacks of cellulitis that are so frequent and so intense, she requires antibiotics every day to keep the infections from occurring.
She had 898 cubic centimeters of excess fluid in her arm. For perspective, 2000 cubic centimeters is a two-liter soda bottle’s worth of volume. So, she has about half of that in one arm alone, which is an enormous amount of fluid.
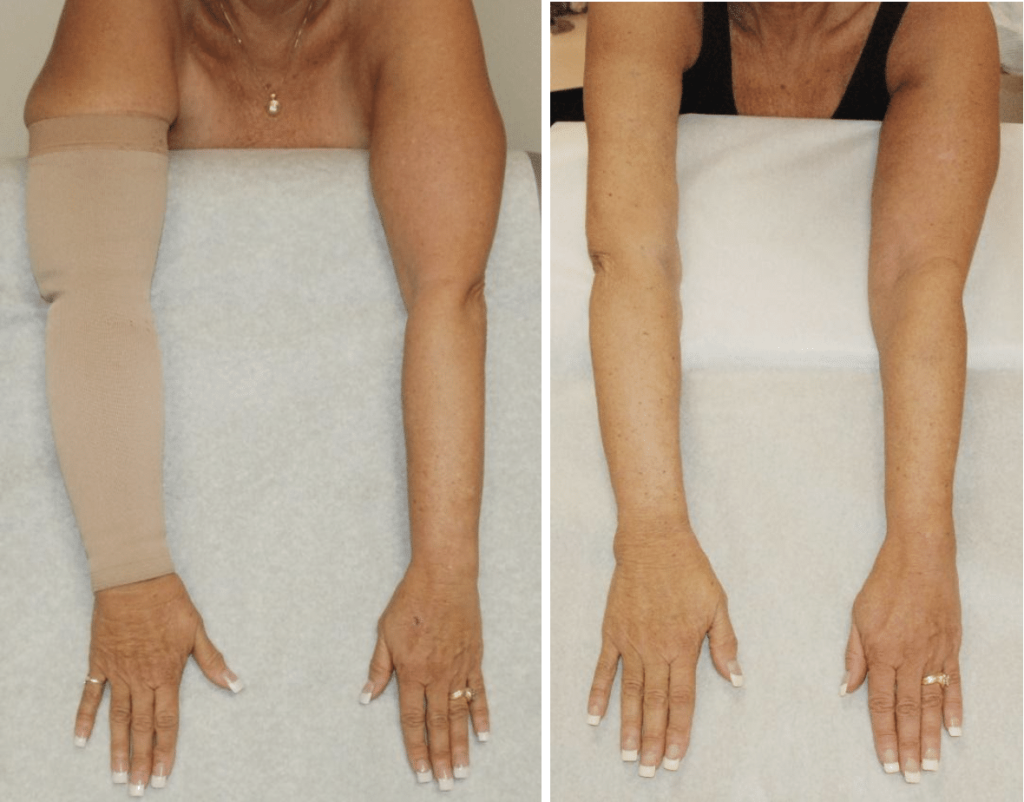
Six months after surgery, the patient’s arm is significantly improved. The reduction is maintained permanently. A photo 18 months after surgery shows that her arm volume reduction is maintained. Her overall results are dramatic, and she no longer needs daily antibiotics. This patient’s quality of life improved tremendously after the surgery.
Granzow SAPLSM Surgery Patient 2:
In another case, a patient with congenital lymphedema had tremendous swelling beginning in her teen years. Since that time, she has not been able to wear jeans or boots. She presented with solid predominant, stage 2 lymphedema where the fluid inflammation has caused permanent solids to form.
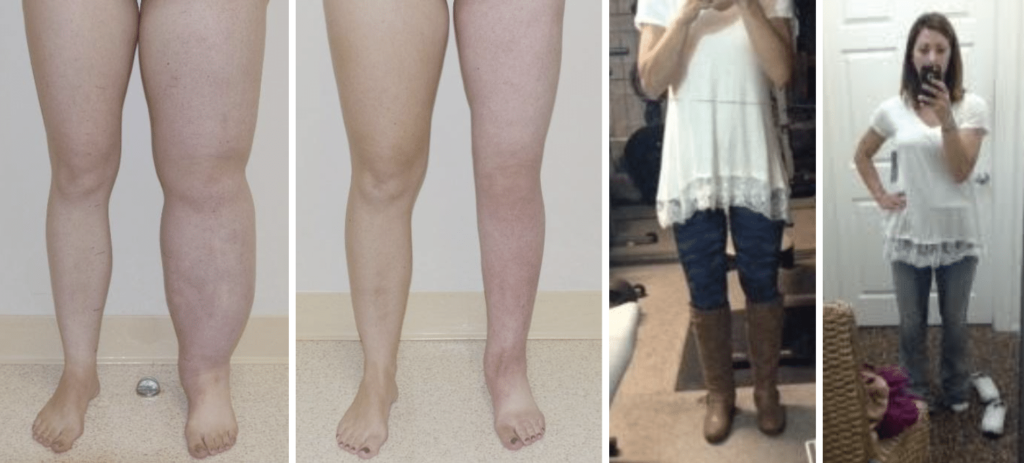
These are results one year after surgery. The patient shared with us that she went shopping in the jean store for the first time, had boots on, and was taking selfies in the department store while she was shopping. It was wonderful to hear how positively the surgery impacted her life.
Granzow SAPL SM Surgery Patient 3:


Here’s another example where the patient had not reached stage 2 lymphedema and was still in stage 1. We caught her early in the progression of her disease when she was using a compression garment daily to manage the lymphedema in her right arm and hand.
Three years after VLNT surgery, she requires no compression garment at all. Some people would say she’s cured of lymphedema, but I prefer not to use the term “cure.” Rather, I would say that this patient has no lymphedema symptoms that disrupt her quality of life. I still recommended to this patient that she takes lymphedema precautions and is careful with her arm during activities.
About Dr. Granzow
Jay W. Granzow, MD, MPH, FACS is an internationally renowned lymphedema and lipedema surgeon, Board Certified in both Plastic Surgery and Head and Neck Surgery. He serves as a Clinical Professor of Surgery in the Division of Plastic Surgery at the UCLA David Geffen School of Medicine. A pioneer in lymphedema and lipedema surgery, Dr. Granzow frequently speaks at U.S. and international conferences and publishes significant scientific articles in leading medical journals. His integrated treatment system achieves long-term results to improve patients’ quality of life.
Share this post
Related Posts...
Explore
Contact Us.
We're ready to help.
Looking for more information, or to be connected with your local representative?
We can help. Fill out our contact form to get started.