By Dr. Emily Iker
Editor’s note: Dr. Emily Iker is the director of the Lymphedema Center in Santa Monica and has a global reputation for her expertise in lymphatic disorders. She’s also one of the co-authors of the Standard of Care for Lipedema in the United States. This is a 10-minute read.
In 1940, lipedema was viewed as disproportional obesity characterized by the bilateral and symmetrical distribution of the fat in legs with swelling in the lower extremities. By 1997, it had become clear that lipedema is a chronic disease with symmetrical impairment of the fatty tissue distribution.
Now, in 2021, phlebology has helped us further define and refine our understanding of lipedema. Today’s definition is as a loose connective tissue disease of the lower extremities with increased nodules of fibrotic adipose tissue. It occurs primarily in women, and in my practice, I have seen only two men display the disorder, but they also had hormonal disturbances and very low levels of testosterone.
We know there is a hormonal influence at play here, as we see the condition primarily in puberty, after pregnancy, and in menopause. It’s also important to note that lipedema involves tissue that’s usually quite painful and hypersensitive to touch, plus it often involves reduced mobility.
Common Comorbidities and Presentation of Lipedema
Lipedema is often misdiagnosed as or is accompanied by conditions like obesity, venous disease, hypermobility of the joints, or diabetes. However, it’s a separate diagnosis of its own.
We also know lipedema tissue is very difficult to reduce through diet, exercise, or even bariatric surgery. One of my patients was 500 pounds before bariatric surgery and while the surgery reduced weight from her upper body, her lower body remained mostly the same.
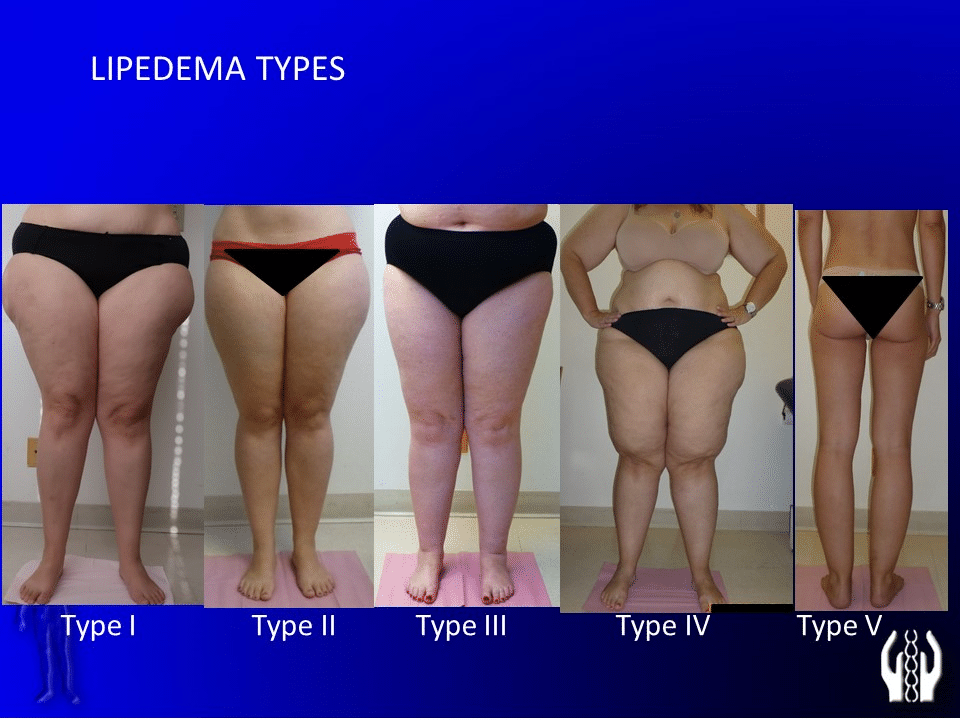
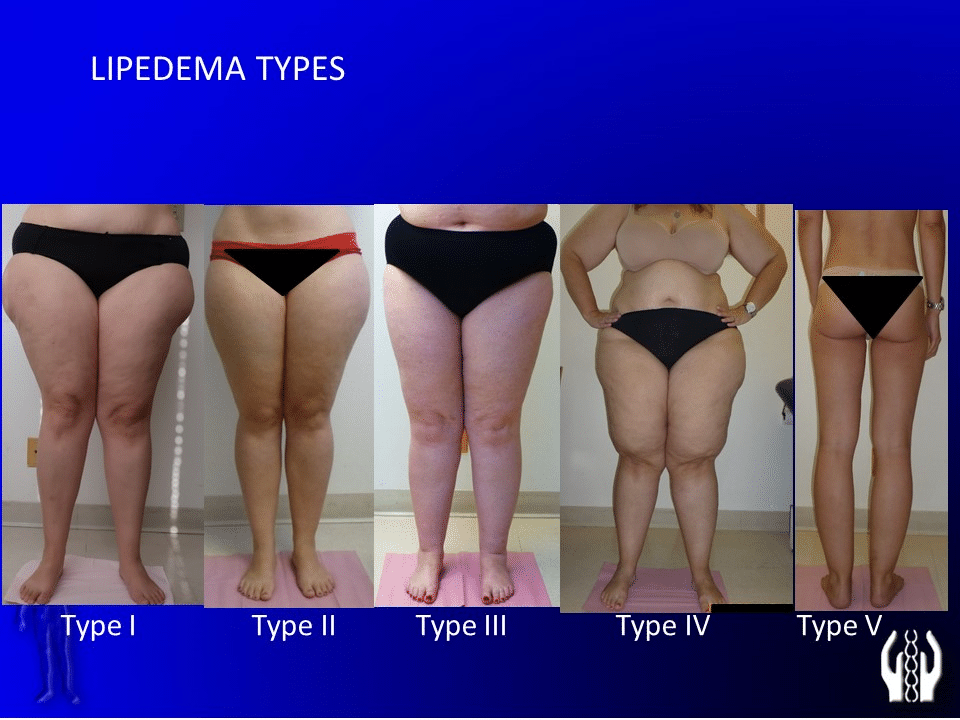
In terms of the diagnostic criteria and coding, lipedema is code EFO2.2 and is characterized by non-pitting diffuse swelling that is usually confined to the lower extremities, legs, thighs, hips, and upper arms.
Biophysiology tells us there is a genetic predisposition to lipedema and about 60% of the population has a genetic makeup from the mother, grandmother, and further on. It’s also polygenic, or influenced by more than one gene from the maternal side.
The estrogen receptors are altered in expression. Subcutaneous fatty hyperplasia and hypertrophy are seen on scans and there is altered adipogenesis and microvascular dysfunction of lymphatic and blood capillaries. This includes increased capillary permeability in endothelial dysfunction, with disturbance of the lymph drainage.
Symptoms of Lipedema From the Patient’s Point of View
When patients arrive for a diagnosis, they will often tell you they have heaviness in their legs and a feeling of tension or crushing by the end of the day. After increased activity, the feeling might be even stronger.
There’s often pain to palpation in the affected area. For example, I had a patient tell me she was experiencing pain whenever her husband embraced her. She felt so painfully crunched, even a hug was unpleasant.
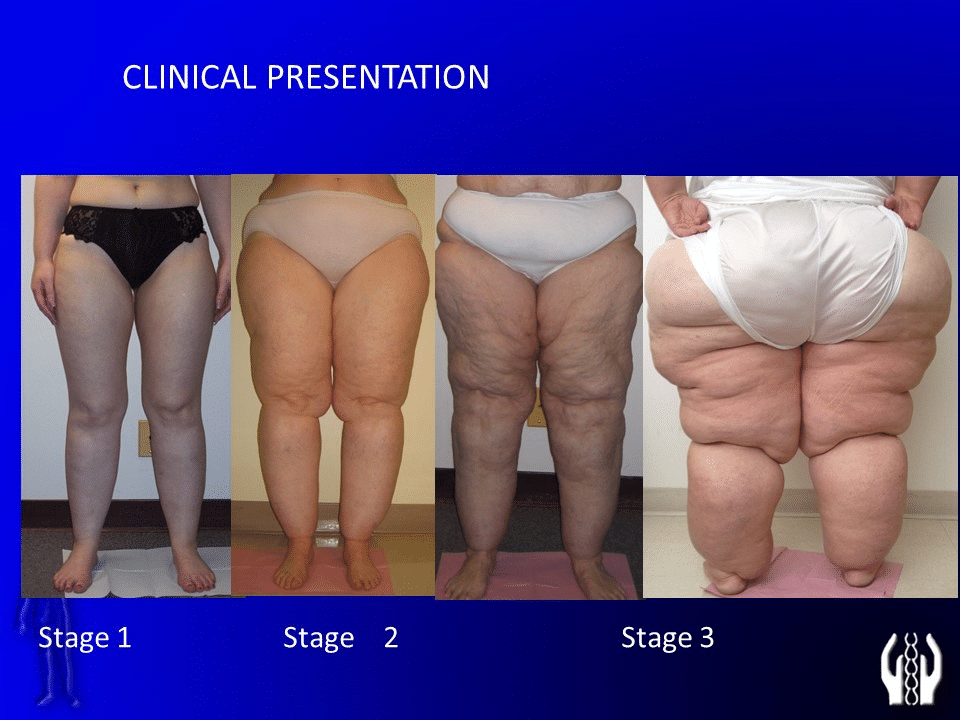
The visual appearance of the affected skin, which should be smooth, is instead spongy and soft. The tissue often has perlite, pea-size, or rice-size subcutaneous nodules. As it progresses, there can be labials with a mattress-like formation of increased spongy swelling.
As the later stages progress, there is no response to elevation. The swelling progresses and remains, regardless of the patient’s attempts to get the swelling down by resting or raising their legs. Later stages are also associated with muscle weakness and impacts on mobility.
Some patients have extreme difficulty with ambulation when there is significant friction between the thighs. The progression of the condition can impact the feet and toes, causing trouble with wearing certain footwear.
I had a patient whose primary complaint was that she couldn’t fit into boots. She’s very slim, but there’s a great disproportion of her lower body extremities, especially below the knee.
Another patient was concerned about the difficulty of finding pants that would fit her. She was a size four in the waist but needed a much different size for her lower body. She’d found a surgeon who tried to give her a consistent body size back through liposuction, but perhaps due to the surgeon’s lack of expertise, this patient was more unhappy after the surgery than before.
Case Studies Show the Importance of Proper Diagnosis and Treatment
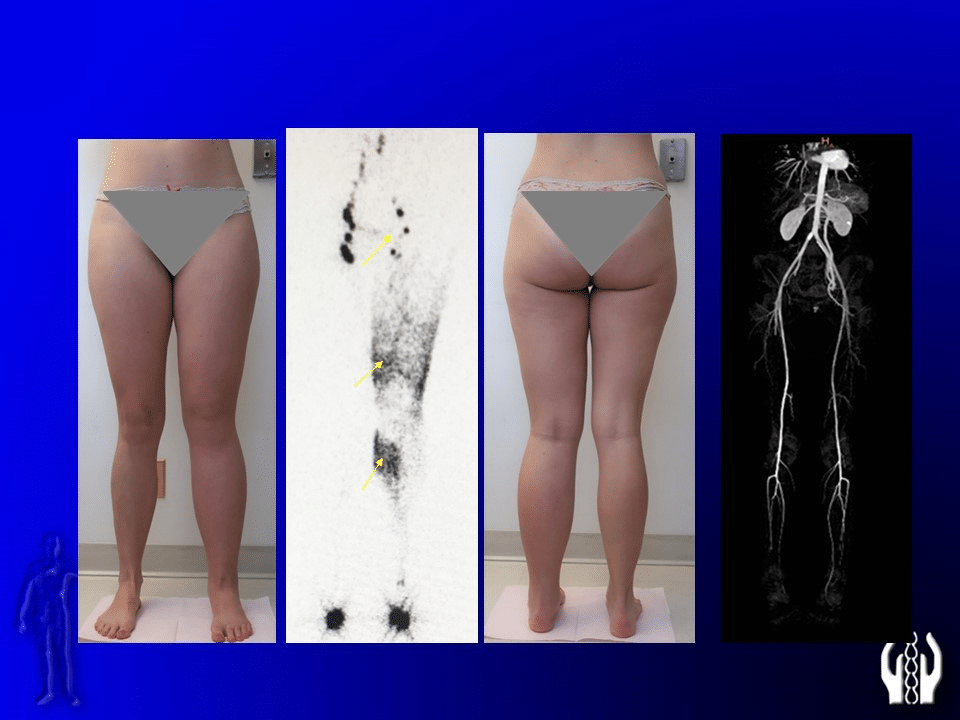
In my practice, I encountered a very interesting 20-year-old female who came to me with symptoms of spontaneous swelling of the left ankle, foot, and toes. She had experienced tension, pressure, and heaviness in her left lower extremity more than her right.
This patient had already been diagnosed with May-Thurner syndrome, which is a vein and artery disorder that creates a high risk of deep vein thrombosis. There’s compression of the left common iliac vein by the right common iliac artery, and this patient’s flow was reduced by 50%.
Stenting can open up the vessels, but this patient’s symptoms continued even after the successful stenting. We did further study, which included visualization of her lymphatic system and discussing the details of her personal history. She’d started with swelling in her distal ankle and foot, which we primarily see with lymphedema patients.
As her symptoms progressed, she not only had heaviness and tension, but also pain to the touch with easy bruising, fatigue, and IBS. She described abdominal or pelvic pain that increased with her monthly cycle.
Her venogram showed indications of pelvic congestion syndrome, a venous condition that causes chronic pelvic pain. What does this tell us? It means that while she came in with an existing diagnosis of May-Thurner syndrome, this was an incomplete picture.
Her case shows the importance of going back to the initial diagnosis and then going even further back, conducting a more rigorous patient history. It also shows the value of a more complete and interactive physical examination, followed by further study and scanning to determine a more accurate diagnosis.
In another case, a 36-year-old woman had delivered a baby about eight months before her visit. After the pregnancy, she tried many types of diet and exercise but was unable to lose any weight. We examined her and found that she had a lack of defined muscle. There was a disparity in her waist to hip ratio and she also had easy bruising of the skin.
For this patient, we tried 30 minutes of Lympha Press treatment to the left lower extremity. On her scan, you could see the interrupted skin and subcutaneous fascia. After one half-hour of therapy with the Lympha Press, the subcutaneous space was reduced by 50%.
Finally, I’d like to address Dercum’s disease, a rare disorder characterized by painful growths of fatty tissue known as lipomas. These growths primarily occur on the trunk, upper arms, and upper legs. The lipomas appear subcutaneously, just under the skin, but also deep within the body in muscles, tendons, ligaments, or even bone.
Patients with Dercum’s disease see improvements with compression garments and the use of pneumatic compression. Like many types of treatment for lipedema, lymphedema, and related disorders, results depend on compliance.
After pneumatic compression treatment, we advise them, “It’s not going to last if you’re non-compliant.” We strongly encourage them to use a compression garment after each treatment to maintain the improvement. Also, it’s important to note that not all pneumatic compression is created equal, and a Lympha Press was used in the study I mentioned earlier.
Compression is a key aspect of managing many of the conditions discussed here. Studies have shown that manual drainage is effective, but isn’t the primary factor in the overall reduction of the fluid volume. Ultrasound studies show compression is much more effective in the reduction of volume and helping patients maintain positive results over the long term.
About Dr. Emily Iker
Dr. Emily Iker is the director of the Lymphedema Center in Santa Monica. She’s known worldwide for her expertise as a physical medicine and rehabilitation specialist who focuses on the diagnosis, management, and treatment of lymphatic disorders. She’s a member of numerous lymphological societies and was certified by A. Leduc, Ph.D., a world-renowned leader in lymphedema research and treatment. Dr. Iker was awarded the Honorary Membership of the Lymphological Association of J.E. Purkyne and is the past president of the American Society of Lymphology. She was also awarded with honorary membership to Slovak Medical Angiological Society, ANNO MMX. On June 8, 2019 Dr. Iker received the lifetime achievement aware for tireless commitment to the treatment of lymphatic disease presented at the 2nd Annual USC Multidisciplinary Lymphedema Symposium in Santa Monica . She is also an international lecturer in lymphology who has a personal understanding of lymphedema.
About Lympha Press
For more than 40 years, Lympha Press has provided innovative compression pump home therapy equipment that supports the best possible patient outcomes.