This is an 11-minute read.
Delving deeper into case histories, we can explore the impact of lymphedema therapy and compression garments and how their use supports the results of lymphatic surgery.
Ideally, post-surgical patients should have access to supportive therapies, including the use of lymphedema therapy and compression garments that contribute to the surgery’s ongoing success. I have treated many patients who have been able discontinue compression garment use following their lymphedema surgeries. However, patients that come to us with more severe damage to their lymphatic systems benefit tremendously from the proper use of lymphedema therapy and compression garments when needed.
Below are a few real-world examples where compression garments work in tandem with surgery to provide the best possible health outcomes for lymphedema patients.
Two-Phase Lymphedema Surgery and Compression Therapy Significantly Help a Patient With Breast Cancer and Chronic Lymphedema
The first patient suffers from 19 years of chronic lymphedema, as well as breast cancer. The patient experienced repeated bouts of cellulitis and took a daily antibiotic to manage infections. Most therapists would define this as a very difficult case to treat.
The patient’s pre-surgical photos show a tremendous amount of swelling. She required continuous around the clock compression garment use to prevent further progression of her lymphedema disease.
She was treated successfully with Granzow SAPLSM surgery. Six months post-surgery, the volume of her arm was considerably reduced such that the affected arm size was about the same as the size of the unaffected arm. This patient has continued to use her compression garment to support the fantastic results of her surgery. The volume reduction persisted 18 months after her procedure and fluid swelling was prevented by her garment.
Subsequently she underwent vascularized lymph node transfer (VLNT) surgery to the left axilla, which reconstructed her lymphatic system. This produced a final 119% overall excess volume reduction and decreased the need for compression to such an extent that she could be out of compression 11 to 15 hours per day.
Reduction in the Need for a Compression Garment
The second patient had lymphaticovenous anastomosis (LVA) surgery, where multiple lymphatic vessels in the affected limb are connected to nearby veins, thus bypassing the damaged area and restoring the flow of lymph fluid into the venous system.
Before her surgery, she would have significant fluid accumulation in the leg. During the surgery, small incisions were made on her leg for the LVA procedure.
In follow-up photos taken 55 months after surgery, volume reduction was maintained with a about 85% less self-care and effort. She can enjoy boating or hiking without a compression garment and her quality of life is greatly improved.
The compression garment still remains and important tool to maintain the reduced volume in her leg at home and at night.
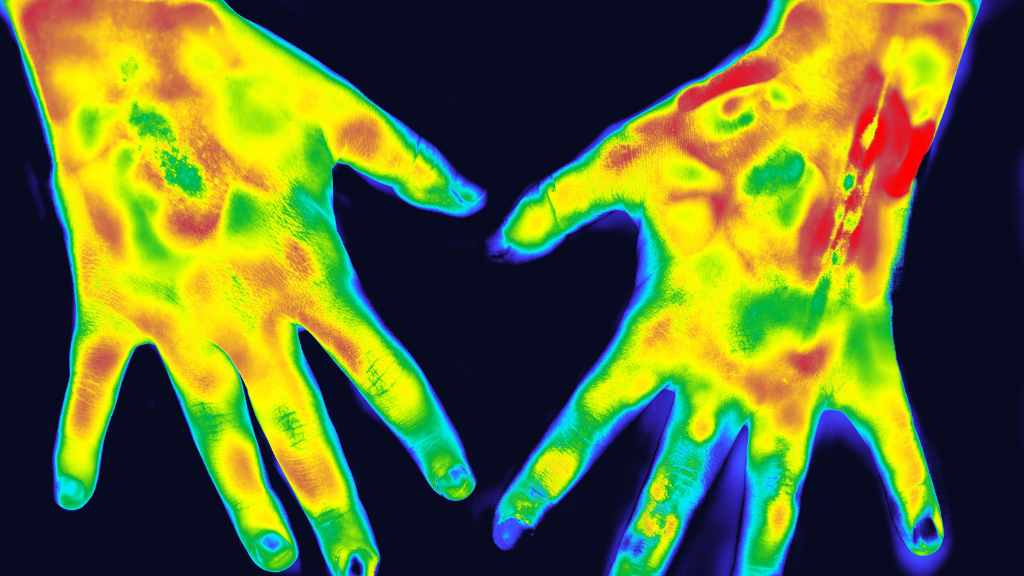
[Figure 2A-B]
A Two-Phase Approach to Chronic Lymphedema Swelling
This patient came to us with a lymphatic system of the left arm that had previously suffered severe damage during treatment for breast cancer surgery. The lymphatic damage was a side effect of the successful breast cancer treatment. The patient had over 1000cc (1 liter) of volume swelling, most of which consisted of pathologic solids such as fat and proteins. She required a class 3 compression garment during the day and a nighttime compression garment to prevent worsening of her condition.
She was treated with Granzow SAPLSM surgery first. This reduced the volume of the arm to approximate the volume of the other arm. A compression garment prevented reaccumulation of the toxic fluid.
She was then treated with VLNT surgery as a second phase procedure to reconstruct the lymphatic system. The VLNT helps her body clear lymphatic fluid every day. With the help of compression therapy, she’s been able to keep the volume buildup down but no longer requires compression during the daytime hours, allowing her to get out and play golf more frequently.
Lymphatic Surgery, Compression Therapy, and Living Life
Before surgery, patients often express concerns about what their life will be like afterward. Will they have scars? Will they be able to play sports and do outdoor activities? Will they still need to wear a compression garment?
In patients with stage 1 lymphedema or the arm or leg, I can borrow extra lymph nodes from the outside part of the groin or the torso and carefully transplant them to the affected area with VLNT surgery. Prior to the VLNT surgery most patients require compression for 23hours or more during the day to prevent worsening of their swelling. After VLNT surgery, patients can reduce the need for the compression during the day significantly.
For a patient who’s a golfer, a tennis player, or does other outdoor activities, this surgery works out wonderfully. They have less reliance on a garment and end up with a small surgical incision in the armpit which heals up well and minimizes any impact on physical activities.
For various reasons, I don’t like to put lymph node transfers into the wrist or ankle, instead moving lymph nodes to the thigh or armpit. With this surgery I can achieve both improved drainage and also improved appearance.
The compression garment plays a key role in this successful outcome. More compression is generally needed in those patients who began the process with greater damage to their lymphatic system.
A Cinderella Story From Compression and Lymphatic Surgery
I’d like to wrap up this article by sharing a story that touched my heart as a lymphatic surgeon. A female patient presented with a severely swollen leg and tremendous damage to her lymphatic system following treatment for ovarian cancer. She been using compression therapy around the clock to manage her condition – more than 23 per day, every day. I determined she was a good candidate for a suction-assisted protein lipectomy surgery, also known as Granzow SAPLSM Surgery.
After a series of surgeries including Granzow SAPLSM surgery, VLNT surgery, and LVA surgery, we were able to make huge strides in reducing the swelling in her right foot and ankle. After the surgeries, she achieved a 109% reduction in fluid volume, which means her affected lymphedema leg actually became slightly smaller than her opposite leg.
As a result, her 23-hour need for compression lowered to just 12 hours per day. This created a dramatic change in her life, allowing her to go many hours without the compression garment, wear nice clothes, attend events, and open up clothing and footwear options that were previously unavailable to her.
She had a pair of shoes she had not been able to wear since before her lymphedema swelling started. Through the years, she had tried on the shoes again and again, but her affected foot would never fit.

After her surgeries and post-surgical self-care, she was finally able to slide both feet into the shoes perfectly. She told me, “today you can call me Cinderella because the right foot fits!”
I love hearing stories like this from happy surgical patients. Whether you’re a lymphedema clinician or a patient, I welcome you to reach out to me and share your stories and questions through my practice’s website at www.lymphedemasurgeon.com.
About Dr. Granzow
Jay W. Granzow, MD, MPH, FACS is an internationally renowned lymphedema and lipedema surgeon, Board Certified in both Plastic Surgery and Head and Neck Surgery. He serves as a Clinical Professor of Surgery in the Division of Plastic Surgery at the UCLA David Geffen School of Medicine. A pioneer in lymphedema and lipedema surgery, Dr. Granzow frequently speaks at U.S. and international conferences and publishes significant scientific articles in leading medical journals. His integrated treatment system achieves long-term results to improve patients’ quality of life.