by Karen Ashforth, MS, OTR/L, CLT-LANA
This is a 9 minute read
Breast Cancer-related Fibrosis: An Evidence-based Update
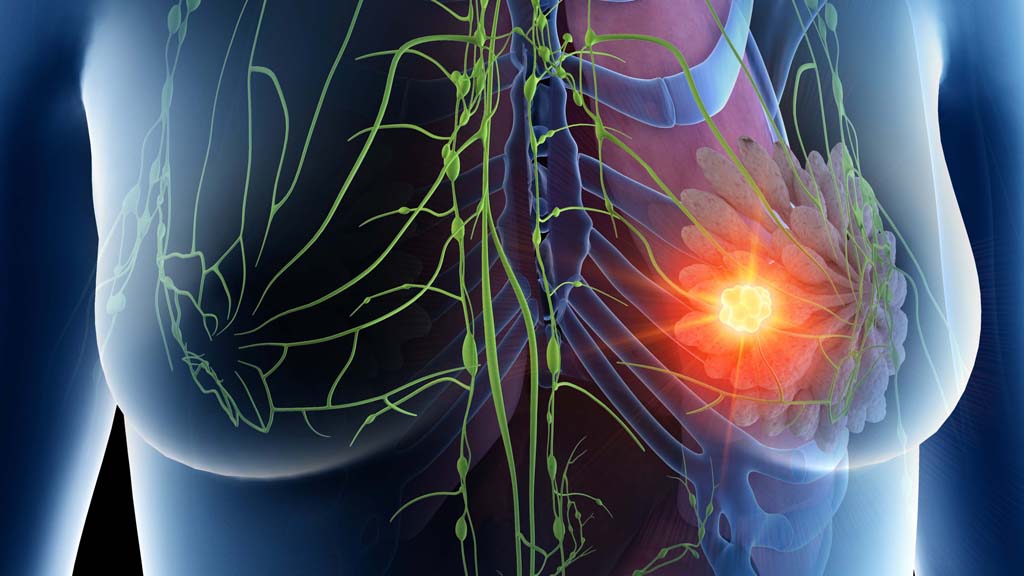
Fibrosis is a process that occurs when healthy tissue is damaged and replaced by hardened and/or thickened tissue. Many identify breast cancer-related fibrosis as surgical scarring or radiation-induced tissue damage, but there are a number of other causes. The most common form of fibrosis is present in all lymphedema: lymphostatic fibrosis. It is important for clinicians to understand, identify, and treat the different types of fibrotic damage that are possible in breast cancer patients, because unaddressed fibrosis directly impacts the severity of lymphedema.
Lymphostatic Fibrosis
Lymphostatic fibrosis is present in all stages of lymphedema, with fibrosclerotic changes occurring even in stage 0. Lymphostatic fibrosis occurs as a result of an inflammatory process triggered by prolonged lymph stasis. The high protein lymph in the extracellular matrix attracts fat cells, which forms a matrix that progressively becomes permanent fatty tissue (Azhar 2020, Földi 2012.) All the other types of fibrosis described in this article can potentially block lymphatic circulation and compound lymphostatic fibrosis.
Post-Surgical Fibrosis
Scar tissue is a common and well-known form of fibrosis in breast cancer treatment. Scar tissue can block lymph drainage, especially if it is greater than 3 mm in width and perpendicular to lymph collectors (Zuther 2018.) In addition to a lumpectomy or mastectomy, lymph node dissection increases risks for lymphedema (Lynch 2015.) Many factors can influence surgical outcomes including the type and extent of surgery, type of surgeon, the patient’s co-morbid inflammatory factors which influence the amount and duration of post-surgical swelling and wound healing, and other treatments such as chemotherapy or radiation therapy that can compound wound and scar healing (Armer 2019, Brahma 2019.) It is important to understand wound healing and how it influences scar formation.
The Stages of Wound Healing
Inflammation and swelling are necessary components of wound healing, but if they are excessive or prolonged, it can delay wound closure and/or affect the scar properties. Wound healing begins with the inflammatory stage that normally lasts for up to 5 days after surgery, when vascular constriction and clotting occurs and neutrophils enter the wound to remove bacteria. The proliferative phase normally occurs between 3 days to 3 weeks after surgery and during this time fibroblasts produce a collagen matrix to repair severed tissues. The final phase of scar maturation normally begins at 3 weeks when the collagen fibers start to align and build tensile strength; this phase lasts up to two years (Wallace 2021, Hu 2016, Wells 2015.)
Post-Surgical Fibrosis Influences
Wound and scar healing is directly influenced by pre- and post-surgical swelling and inflammation and there are many factors that influence the severity and duration of this process.
Patients with lymphedema prior to surgery, or who develop post-surgical lymphedema have lymphostatic fibrosis, which can lead to a vicious cycle of increased inflammation, increased lymphatic circulation impairment, and increased lymphostatic fibrosis. (Azhar 2020)
Comorbidities influencing post-surgical inflammation include obesity, diabetes, circulatory or autoimmune conditions. There are a myriad of medications with inflammatory side effects that include antidepressants, anti-diabetics, immunosuppressants, calcium channel blockers, anti-neuralgics, and taxane-based chemotherapy. Even NSAIDS and corticosteroids commonly prescribed for post-surgical pain can have inflammatory side effects (Keeley 2020.)
Post-surgical complications can lead to additional types of fibrosis: seromas (Ouldamer 2016, Van Bemmel 2011), cellulitis infections (Burian 2021, Chlebicki 2014), non-healing wounds (El Ayadi 2020) and tissue necrosis (Jagsi 2107, Khansa 2013) can create permanent tissue damage that further disrupts circulation. Surgical scarring can be aggravated by a genetic predisposition to keloid scar formation (Andrews 2016.) Untreated pre- or post-surgical lymphedema produces lymphostatic fibrosis. Radiation therapy is damaging to tissues, and can be especially damaging to scar tissue, particularly if wound healing has been delayed or if the scarring is hypertrophic.
Radiation-induced Fibrosis
Radiation therapy alters tissue composition, making tissues thinner, harder and more brittle. Radiation following surgery creates changes to the surgical scar to make it harder and denser, as well as creating fibrotic tissue around the scar. Some of the mechanical factors that influence radiation damage include: type, duration, intensity, amount, and location of the radiation field. There are also patient-oriented factors that affect tissue healing and long-term outcomes such as skin sensitivity, tissue density and composition. In addition to damaging the skin, late effects of radiation therapy can create significant damage to organs and other internal tissues, producing heart disease, neuropathy, osteoporosis and even tooth loss (DiFrancesco 2020, Kline-Quiroz 2019, Purkayastha 2019.)
Cording
Cording, also known as Axillary Web Syndrome, can be a painful and debilitating form of fibrosis. Cording can feel and appear like one or more guitar strings just under the surface of the skin, and occurs most commonly between the axilla and the antecubital fossa of the elbow, although cords can extend down into the hand or the trunk. Recent research has shown cording has been associated with lymph vessel impairment: either thrombosis or impaired pumping action due to proinflammatory conditions, resulting in dermal backflow. This could explain why sometimes cording spontaneously reverses, and in other cases, persists (Malek 2021, Koehler 2020, Andrews 2016.)
Fibrosis Treatment Options for Breast Cancer Patients
Prior to treating fibrosis, it is important to address swelling. Superficial congestion can obscure deeper fibrotic tissue, making it more difficult to treat. Complete decongestive treatment of manual lymph drainage, compression, skin care, and exercise form an important foundation for fibrosis treatment by giving patients tools to deal with swelling, and prevent the progression of lymphedema and fibrosis.
Treatment for lymphedema and fibrosis frequently overlap, but many fibrosis treatments are too intense to use with vulnerable tissues immediately following surgery and radiation therapy. Gentle treatment is more appropriate while the body takes time to heal sufficiently. If the patient has also had chemotherapy, the body needs an even longer period of healing time to allow the immune system to recover before starting any type of aggressive fibrosis treatment.
Treatment Example: Breast Cancer Related Lymphedema and Fibrosis
This case example describes many of the types of lymphedema and fibrosis treatments commonly used to help a breast cancer patient.
A.M. had neoadjuvant chemotherapy and then underwent a right breast lumpectomy with axillary node dissection (2/12 nodes positive for cancer.) Four weeks post-surgery, she was referred to lymphedema therapy because of worsening swelling of her right arm, axilla, thorax and breast and her surgeon wanted swelling resolved quickly because radiation therapy was planned.
A.M. received a comprehensive lymphedema evaluation and began Complete Decongestive Treatment. Her lymphedema therapist performed manual lymphatic drainage while using a low-level laser (Bell 2018, Carati 2003) to help with wound and scar healing, and taught A.M. self-MLD. She performed arm bandaging as well as recommending A.M. wear a post-surgical bra with soft prosthesis over a chip foam breast/thorax pad to compress her right breast, axilla and thorax both night and day. She also recommended the use of a silicone scar gel pad to influence collagen maturation and flatten the raised surgical scars (Goldberg 2016, Bleasdale 2015.) She instructed A.M. in lymphedema risk reduction and infection prevention, in arm elevation and in shoulder range of motion exercises. After three weeks of bandaging, A.M. transitioned to wearing a Velcro wrap on her right arm and a compression glove on her right hand during the daytime, and a quilted chip foam arm sleeve nocturnally.
A.M. began radiation therapy, and applied cream to the tender skin on her breast and axilla that was provided by her radiation oncologist. She wasn’t able to tolerate wearing thoracic compression the last few weeks of treatment because her skin was irritated from the radiation desquamation effects.
Despite daily conservative treatment, A.M. continued to demonstrate significant right upper quadrant swelling, and her therapist recommended a pneumatic compression device. Using this specialized lymphedema pump created compression, decongestion and softening of the tissues of her arm, axilla, breast, and thorax. A.M. wore her quilted garments while using the pump to create a “dual massage” which furthered the softening of fibrotic tissue and reduction of the swelling in her entire right upper quadrant. This helped her to progress from using the Velcro arm wrap to a custom flat knit arm compression sleeve with an antifibrotic weave, which created a mild micro-massage while she wore it. A.M.’s swelling was finally under control with her home compression program and she stopped seeing her lymphedema therapist.
Several months later, A.M.’s breast and thorax had completely healed from radiation therapy and her hair had grown back from chemotherapy. But the skin and underlying tissue of her breast, thorax, and axilla was getting thicker and harder and A.M. returned to her lymphedema therapist, who recommended quilted cherry pit pads to use in addition to her quilted chip foam garments as a more aggressive anti-fibrotic treatment to target softening of tissues on her breast and axilla areas (Ashforth 2011.) Her therapist also used the low-level laser over these areas while performing anti-fibrotic massage with specialized instruments (Seffrin 2019, Kim 2017) along with negative pressure to lift and stretch her hardened tissues (Gott 2018, Jamalian 2017.) Her therapist performed a trial in the clinic with A.M. to titrate and increase the pressure on her pneumatic device within comfort levels to increase the anti-fibrotic effects.
A.M. started to feel so much better that she felt ready to join an aquatic decongestion class that was sponsored by her lymphedema clinic. Being in the water helped her swelling and as she built up her stamina and could exercise more, she lost weight, which helped to further decrease her lymphedema and fibrosis symptoms.
A.M. continued to use her decongestive and anti-fibrotic tools independently at home and saw her lymphedema therapist for a few visits every six months to upgrade her compression garments, which became loose as she continued to gradually lose weight. She also received “fibrosis tune-up treatments” from her therapist, knowing that her surgical and radiation scar tissue could continue to mature during the two-year window of wound healing.
Although this case describes a patient during and immediately after cancer treatment, I see many patients who completed treatment 10, 20, and even 30 years ago who are just now being referred for lymphedema. While early treatment always yields the best results because it can prevent the progression of lymphedema and fibrosis, I want to give patients and therapists hope: it is my clinical experience that treatment at any stage can help the body heal, improve symptoms, remodel and soften fibrosis, and empower patients with knowledge and tools to self-manage symptoms.
————————————————————
Karen Ashforth, MS, OTR/L, CLT-LANA has practiced as an occupational therapist for over 40 years. Specializing as a board-certified hand therapist led to her interest and specialization of treating lymphedema and fibrosis 20 years ago.
Karen’s passions in lymphedema practice are equipment innovation and development, treatment of underlying fibrosis and inflammation, and assessment of complex and difficult cases. She is considered an expert in clinical use of pneumatic compression and has participated in the development of numerous devices and appliances. She has outpatient lymphedema practices at St. Joseph’s Medical Center in Stockton, California, and Dominican Rehabilitation in Santa Cruz, California, as well as a private telehealth and consulting practice.
Karen speaks frequently at academic, clinical and professional settings and performs clinical research that she presents and publishes nationally and internationally. She is also an adjunct faculty member with the University of the Pacific in the Doctoral Physical Therapy Program.
LEARN MORE: LIVE WEBINAR – OCTOBER 27, 2021 12:30 PM EST
NOTE: This presentation and all webinars in the Lympha Press Education Series are recorded. Registrants will receive a link to watch the replay at their convenience. For those who wish to ask questions of the presenter, we encourage attending the live event.
References:
Andrews JP, Marttala J, Macarak E et al (2016) Keloids: the paradigm of skin fibrosis – pathomechanisms and treatment. Matrix Biol 51: 37-46.
Armer J, Ballman K, McCall L (2019) Factors associated with lymphedema in women with node-positive breast cancer treated with neoadjuvant chemotherapy and axillary dissection. JAMA Surgery doi:10.1001/jamasurg.2019.1742.
Ashforth K, Morgner S, VanHoose L (2011) A new treatment for soft tissue fibrosis in the breast. Journal of Lymphoedema 6(2): 42-46.
Azhar SH (2020) The unresolved pathophysiology of lymphedema. Frontiers in Physiology 11:137. doi: 10.2289/fphys.2020.00137.
Bell L, Stout NL (2018) Using low level light laser in your lymphedema practice: benefits and cautions. Rehabilitation Oncology 36(1): 70-72.
Bleasdale B et al (2015) The use of silicone adhesives for scar reduction. Advances in Wound Care 4(7):422-430.
Brahma B, Yamamoto T (2019) Breast cancer treatment-related lymphedema (BCRL): An overview of the literature and updates in microsurgery reconstructions. European Journal of Surgical Oncology 45: 1138-1145.
Burian EA et al (2021) Cellulitis in chronic edema of the lower leg: an international cross-sectional study. British Journal of Dermatology 185:110-118. doi: 10.1111/bjd.19803
Carati CJ, Anderson SN, Gannon BJ, Piller NB (2003) Treatment of post-mastectomy lymphoedema with low level laser therapy: a double blind, placebo controlled trial. Cancer 98:1114–22.
Chlebicki MP, Oh CC (2014) Recurrent cellulitis: risk factors, etiology, pathogenesis and treatment. Curr Infect Dis Rep 16:422 DOI 10.1007/s11908-014-0422-0
DiFrancesco T, Khanna A, & Stubblefield, MD (2020). Clinical Evaluation and Management of Cancer Survivors with Radiation Fibrosis Syndrome. Seminars in Oncology Nursing, 150982.doi: 10.1016/j.soncn.2019.150982
El Ayadi A et al (2020) Current approaches targeting the wound healing phases to attenuate fibrosis and scarring. International Journal of Molecular Sciences 21, 1105; doi:10.3390/ijms21031105.
Földi M, Földi E (2012) Treatment of lymphostatic fibrosis. In: M Földi, E Földi, S Kubik, (Eds.) Textbook of Lymphology for Physicians and Lymphedema Therapists (p. 484). 3rd ed. Munich: Urban & Fischer.
Garza R, Skoracki R, Hock K et al (2017) A comprehensive overview on the surgical management of secondary lymphedema of the upper and lower extremities related to prior oncologic therapies. BMC Cancer 17:468 doi:10.1186/s12885-017-3444-9.
Goldberg D (2016) Efficacy and safety of a novel 100% silicone scar gel treatment for early intervention in scar management. Journal of Clinical and Aesthetic Dermatology 9(12): 13-20.
Gott et al (2018) Negative pressure therapy in the management of lymphoedema. Journal of Lymphoedema. 13(1): 43-48.
Hu MS, Longaker MT (2016) Dipeptidyl peptidase-4, wound healing, scarring and fibrosis. Plastic Reconstr. Surg. 138(5): 1026-1031.
Jagsi R et al (2017) Complications after mastectomy and immediate breast reconstruction for breast cancer: a claims-based analysis. Ann Surg 263(2): 219-227.
Jamalian S et al (2017) Demonstration and analysis of the suction effect for pumping lymph from tissue beds at subatmospheric pressure. Sci Rep. 7(1): 12080.
Johansson K, Chong H, Ciornei CD, et al. (2020) Axillary web syndrome: evidence for lymphatic origin with thrombosis. Lymphatic Res Biol 18:329–32.
Keeley, V (2020) Drugs and Breast Cancer–Related Lymphoedema (BCRL): Incidence and Progression. Current Breast Cancer Reports.doi:10.1007/s12609-020-00379-8
Khansa I et al (2013) Fat necrosis in autologous abdomen-based breast reconstruction: a systematic review. Plastic and Reconstructive Surgery 131(3): 443-452.
Kim J, Sung DJ, Lee J (2017) Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: mechanisms and practical application. Journal of Exercise Rehabilitation 13(1):12-22. /doi.org/10.12965/jer.1732824.412.
Kline-Quiroz C, Nori P, Stubblefield, MD (2019) Cancer Rehabilitation. Medical Clinics of North America. doi: 10.1016/j.mcna.2019.10.004
Koehler LA, Hunter DW. (2016) Lymphspiration: the axillary web and its lymphatic origin. Lymphology 49: 185–91.
Lynch LL, Mendez U, Waller AB et al (2015) Fibrosis worsens chronic lymphedema in rodent tissues. Am J Physiol Heart Circ Physiol 308: H1229-H1236.
Malek AE, Fife CE, Rasmussen JC et al (2021) Lymphatic dissemination and axillary web syndrome in primary cutaneous tuberculosis secondary to needlestick injury. Open Forum Infectious Diseases doi: 10.1093/ofid/ofab160
Ouldamer L et al (2016) Dead space closure with quilting suture versus conventional closure with drainage for the prevention of seroma after mastectomy for breast cancer (QUISERMAS): protocol for a multicentre randomised controlled trial. BMJ Open (6(4) doi: 10. 1136.bmjopen-2015-009903.
Purkayastha A, Sharma N, Sarin A, et al (2019) Radiation Fibrosis Syndrome: The Evergreen Menace of Radiation Therapy. Asia Pac J Oncol Nurs 6: 238-45.
Seffrin C et al (2019) Instrument-assisted soft tissue mobilization: a systematic review and effect-size analysis. Journal of Athletic Training 54(7): 808-821.
Van Bemmel AJM et al (2011) Prevention of seroma formation after axillary dissection in breast cancer: a systematic review. European Journal of Surgical Oncology 37(10): 829
Wallace HA et al (2021) Wound healing phases. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; accessed from: https://www.ncbi.nlm.nih.gov/books/NBK470443/.
Wells A, Nuschke A, Yates CC (2015) Skin tissue repair: matrix microenvironmental influences. Matrix Biol 49: 25-36.
Zuther, J & Norton S (2018) Complete Decongestive Therapy. In Lymphedema Management: The Comprehensive Guide for Practitioners 4th ed (p.80). Stuttgart: Georg Thieme Verlag.