No products in the cart.
Explore
Contact Us.
We're ready to help.
Looking for more information, or to be connected with your local representative?
We can help. Fill out our contact form to get started.

27
Jun
Are You Using Patient-Centered Functional Outcome Measures for Lymphedema and Lipedema?
This is a 12-minute read.
By Molly Sleigh, OTD, OTR/L, CLT-LANA
Outcome measures can be grouped into four categories: self-report, performance-based, observer-reported, and clinician-reported. These are the four most commonly used categories most clinicians are familiar with.
There is increasing awareness of the need for disease-related, patient-reported outcome measures (PROMs). PROMs are measures of patients’ health-related quality of life (HRQOL), and they add a richer, fuller understanding of the full impact of lymphedema and lipedema on patients’ lives.
Types of Outcome Measures
Performance-Based Measures
Taking a closer look at each category of outcome measures, we see that performance-based measures require patients to complete functional tasks, and scoring is usually based on some type of objective measurement. For example, this measurement might include the time it takes to complete a task.
A qualitative assessment can also be used to assign a score. For example, a qualitative assessment of task performance might include the description of normal or abnormal use of body mechanics while completing that task. Physiologic factors can also be identified during the task performance. These might include tone, balance, weakness, or impaired active range of motion.
The Timed Up-and-Go test is an example of a performance-based measure that any therapist in our field would be very familiar with. It’s a functional mobility test that identifies mobility and balance impairments in older adults as they rise, walk approximately 10 feet, and turn around 180 degrees to come and sit back down.
Another example is the Six-Minute Walk Test, a submaximal exercise test that assesses aerobic capacity and endurance. This demonstrates how well the client can handle six minutes of walking on a hard, flat surface; most of us have probably used it within our clinics.
Observer-Reported Measures
Observer-reported measures are typically completed by someone that has regular involvement or contact with the patient, such as a caregiver or a parent. This person can report behaviors and events related to the patient’s health condition.
An example of an observer-reported measure would include whether or not the patient remembers to complete tasks of daily living. Did the patient forget to turn off the stove? Can he or she recall where their keys are? Does the patient remember how to get to the store?
Observer-reported measures can also be used to capture sequencing ability. For example, does the patient appropriately button their shirt when getting dressed? Is he or she able to put on their stockings correctly? Does the patient seem to experience agitation when trying to accomplish sequential tasks like these?
Clinician-Reported Measures
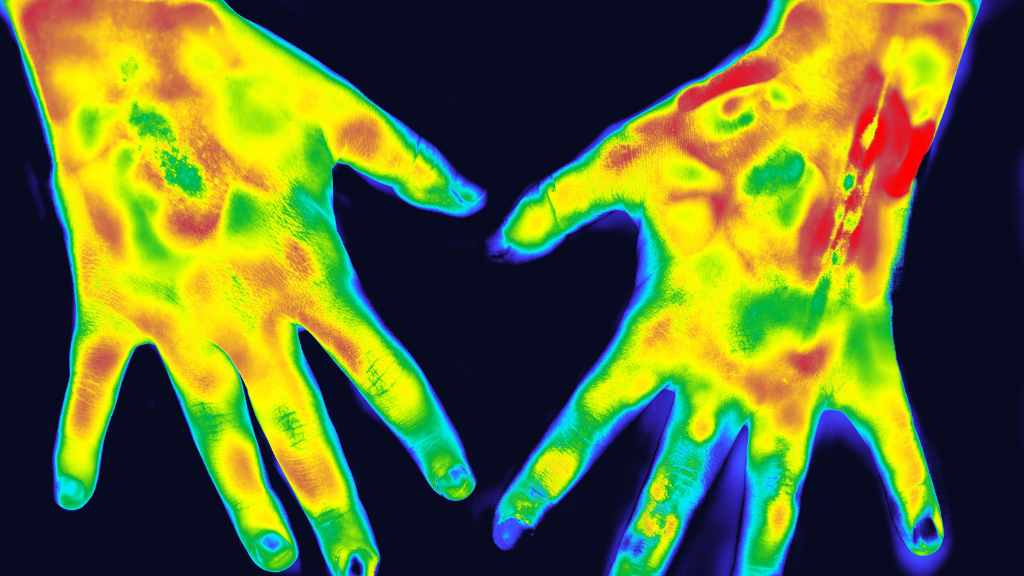
Clinician-reported outcome measures are typically completed by the therapist or healthcare professional using their clinical judgment. They might calculate limb volume, assess the skin, observe pitting edema, measure wounds, and so forth.
Self-Reported Measures
The final category is our primary focus here: self-reported measures. These are the patient’s observations about their own condition. These self-reported measures are important because they help capture what’s important to the patient and how their beliefs impact their condition.
The Importance of Self-Reported Measures
Patient-reported outcome measures are typically captured in questionnaire form and show the psychometric properties of having a certain condition. When examining the effectiveness of a self-report tool, we need to go back and examine the psychometric properties. Psychometric properties are the intrinsic properties of an outcome measure. They should have been tested and developed through a series of rigorous research studies.
A measure with high validity is consistently and reliably able to measure its intended focus. High inter-rater reliability means two different therapists would determine a similar score on a patient performance test. Another aspect, intra-rater reliability, involves serial testing, and no changes are noted without intervention. This is similar to test-retest reliability.
Responsiveness is the ability of the measure to capture a change in status. Please note that there is a ceiling effect here, meaning when the test is too easy, it doesn’t adequately capture the patient’s full ability. There is also a floor effect that occurs when the test is far too difficult and lacks the easier-to-accomplish items that would reveal the patient’s status.
The minimal clinically important difference (MCID) is essential to keep in mind here. This is the amount of change that is relevant from the patient’s perspective. It is a highly important clinical change.
Use of a patient reported outcome measure (PROM) helps clinicians capture disease-specific symptoms within the patient population. When it’s used along with other objective criteria and outcomes, we can more fully observe changes in patients’ conditions that involve disease detection, disease progression, and actual improvement.
PROMs for Lymphedema and Lipedema
Unfortunately, there is an overall lack of published literature relating to the validity of patient-reported outcome measures for lymphedema and lipedema. For this reason, I’d like to highlight a study that was published in 2021 that compared five different outcome measures specific to lymphedema and lipedema.
This study examined the convergent, divergent, and discriminant validity of a set of five instruments in both lymphedema and lipedema. The five outcome instruments utilized were the Short Form 36 (SF-36), Freiburg Quality of Life Assessment of lymphatic disorders, Short Version (FLQA-lk), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Symptom Checklist-90-revised (SCL-90R), and the Six-Minute Walk Test (6-MWT).
What was interesting about this study is that the authors concluded that nine sections taken from each of these outcome measures should be used with every patient in the clinic. I read this conclusion and thought, “How is that even possible for the everyday clinician?” Therapists typically do not have time within 60 minutes to administer so many aspects of so many outcome measures.
In reality, there must be an easy way for the patient to share their reported outcome measures quickly. It’s important to use a very disease-specific quality of life outcome tool or even a limb-specific tool that provides a high level of specificity.
The patient complaints between upper and lower-limb lymphedema are quite different. Individuals with leg lymphedema are hospitalized more frequently, are more likely to have cellulitis, and generally report a worse quality of life than those with upper limb lymphedema.
This illustrates the fact that there are such vast differences between two different areas of the body, it would be most efficient and effective to have a different measurement tool for each. In my practice, I use four main measurement tools to measure outcomes in seven categories. These are discussed in more detail below.
Studies and Categories for Comparison of Outcomes
There are seven key categories for comparison among various patient-reported outcome measures: psychological stress, edema, and financial strain, skin condition, movement/range of motion, activities of daily life (ADL), sexual function, and leisure activities.
Psychological Distress
Psychological distress is especially important because studies demonstrate that higher levels of psychological burden or stress are correlated with a lack of knowledge about their condition. Identifying psychological stress tells us something about how much they may know about their condition.
This is an opportunity for education. The therapist is in the position to communicate self-management strategies that will help the patient minimize their stress and maximize the possibility of positive outcomes.
Edema and Financial Strain
The category of edema and financial strain is also important to highlight due to the significance of financial stability on health and wellness. Financial strain is a significant factor in health-related quality of life and a lack of funds is a potential psychological stress factor.
Skin Condition
The patient’s perception of skin condition and understanding of good skin care is important. It’s known that cellulitis episodes can worsen lymphedema status and lead to a decreased HRQOL. It’s also known that skincare is a key aspect of prophylactic behavior that prevents skin infection.
Movement/Range of Motion
Surprisingly, many patient-reported outcome measures lack questions about movement restrictions or active range of motion. This is concerning because limb heaviness is well-known as a contributor to active range of motion impairment and can be a side effect of both lymphedema and lipedema. Fortunately, ADLs are frequently included in patient-reported outcome measures due to the importance of assessing how well people can independently complete tasks of daily living.
Sexual Function
In regard to sexual function, patient-reported outcome measures can involve the use of a drawing where the patient can shade in or draw the areas where they have edema or swelling. This helps ease the embarrassment of communicating verbally and prevents anxiety or reluctance to report symptoms.
Leisure Activities
Questions about leisure activities should be included. The patients’ answers can be quite revealing in terms of how much their condition is impacting their quality of life and how they perceive living with their disease.
Providing Patient-Centered Care
In summary, the inclusion of patient perception with objective data is very important because it captures more than just what’s important to us as clinicians. It captures what is meaningful to the individual human being involved and reminds clinicians what we’re here for: the patient.
Our patients should always be at the center of our care. The goal of therapy should always be to accomplish meaningful improvements for the patient and take strides to provide what they perceive as an improved quality of life.
About Molly Sleigh
Molly Sleigh, OTD, OTR/L, CLT-LANA, is an adjunct professor in the Department of Occupational Therapy at Rocky Mountain University and an occupational therapist at Centura Health in Colorado Springs, CO. Her educational background includes Concordia University Wisconsin, Rocky Mountain University, and the Academy of Lymphatic Studies, and she is board certified in the treatment of lymphedema through the Lymphology Association of North America. She’s a co-author of the national treatment guideline initiative for the U.S. Lipedema Standard of Care and is a renowned lecturer at the state and national levels on topics including lymphedema, lipedema, venous disorders, lymphatic disorders, and oncology rehabilitation.
About Lympha Press
Lympha Press offers pneumatic compression devices that improve lymphatic flow within the body. If you are a doctor treating patients with lymphedema, CVI, chronic wounds, or lipedema, please take a look at the innovative therapy options from Lympha Press. Our products offer significant relief and are backed by clinical studies.
Share this post
Related Posts...
Explore
Contact Us.
We're ready to help.
Looking for more information, or to be connected with your local representative?
We can help. Fill out our contact form to get started.