No products in the cart.
Explore
Contact Us.
We're ready to help.
Looking for more information, or to be connected with your local representative?
We can help. Fill out our contact form to get started.
12
Jun
Understanding and Treating Truncal Lymphedema
This is a 10-minute read.
The lymphatic system plays a major role in supporting immune system function and balancing fluid levels throughout the body. It does this by utilizing a system of small, thin tubes called lymphatic vessels to collect a colorless, watery fluid throughout the body and return it to the blood vessels. This fluid is called lymph and is packed with white blood cells called lymphocytes.
In addition to this system of vessels and fluid, the lymphatic system includes glands called lymph nodes. These glands have the important job of housing lymphocytes and filtering the lymph fluid by removing damaged or cancerous cells.
When individuals are born with or incur damage to their lymphatic system, it can become difficult for the body to process and manage fluids effectively. As a result, there can be a chronic build-up of fluid, or swelling, in one or more areas of the body, leading to a diagnosis of lymphedema.
Lymphedema is a chronic disease of the lymphatic system that leads to significant swelling in one or more parts of the body. In some patients, the areas affected by lymphedema include the trunk.
What Is Truncal Lymphedema?
Truncal lymphedema specifically involves swelling in one or more areas of the trunk of the body. Little research exists specifically examining truncal lymphedema and its prevalence; however, it is believed that truncal lymphedema is often underdiagnosed.
Truncal lymphedema can lead to discomfort and pain, particularly in the shoulder, chest wall, or back. It may include swelling in the affected breast or chest wall, as well as swelling over the collarbone, under the arm, along mastectomy scar lines, or between scar lines from biopsies, drain sites, or surgeries. The condition can also cause swelling in the lateral trunk, shoulder blades, or back. Truncal lymphedema may also cause sensations of heaviness, fullness, or tingling. In some cases, the swelling can be so significant that it alters the body stance and causes lower back pain.
The likelihood of developing truncal lymphedema is hypothesized to be closely tied to individual anatomy and the location of lymph nodes and lymphatic vessels impacted by treatment or surgery. Lymphedema appears to commonly affect people who have undergone radiation treatment for cancer. An estimated 25-50% of people who undergo radiation or surgical interventions for breast or lung cancers in particular are at an increased risk for developing truncal lymphedema. Some resources suggest that 13% of people with breast cancer who undergo treatment develop truncal lymphedema. Others estimate as many as 35% of people with breast cancer will develop truncal lymphedema, with or without concurrent swelling of the arm.
How to Manage Truncal Lymphedema
Often, symptoms of truncal lymphedema respond well to usual compression and complete decongestive therapy (CDT) approaches used for lymphedema management. Specifically, manual lymphatic drainage (MLD) may be performed by your certified lymphedema therapist (CLT) focusing on all areas of the trunk (chest, breast, back, and inguinal nodes) to improve lymphatic drainage. During treatment, CLTs should begin educating patients and caregivers on performing self-MLD and other self-massage techniques so they can feel confident using these strategies at home.
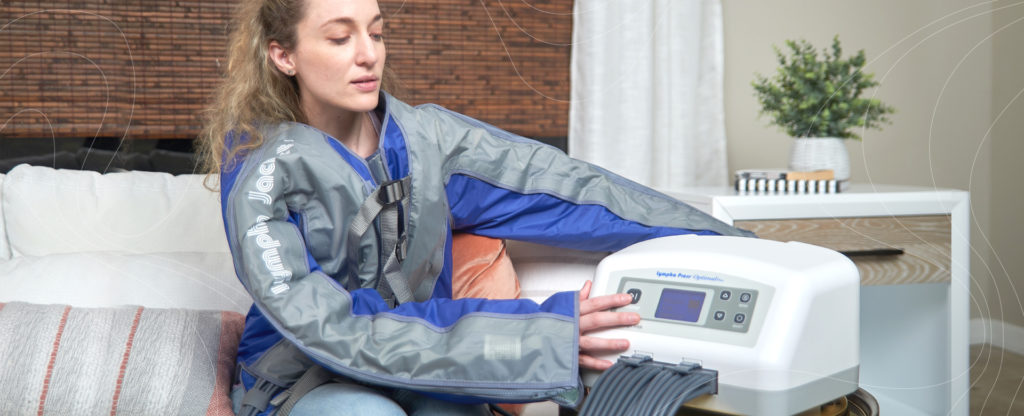
Pneumatic compression therapy can also be used to effectively treat the symptoms of lymphedema at home. Patients are using pneumatic compression therapy garments like the ComfySleeveTM and Lympha JacketTM for targeted upper body truncal lymphedema treatment including side or bilateral treatment of the arms, chest, shoulders, back, and abdomen.
Physicians and CLTs help determine if patients are candidates for compression garments to support truncal lymphedema management and how to best apply these garments for maximum positive effect. While traditional bandaging of the chest, breast, and back is possible, it can be difficult to keep bandaging in place during daily life since the trunk is engaged in all activities. Specialty garments are often a better option to provide appropriate, yet functional, truncal compression.
Exercise is commonly recommended to help treat and manage lymphedema. Physical activity encourages circulation of blood and lymph to improve lymphatic drainage and reduce swelling. This may also help to manage a healthy weight, as being overweight may exacerbate lymphedema-related symptoms. It is important to consult a physician and lymphedema care team members before starting a new exercise program. They will provide information about specific types and pacing of exercises that are safe to perform while managing lymphedema.
Finally, some simple lifestyle changes may manage lymphedema symptoms. Examples of daily life habits to consider include:
- Perform light range of motion movements throughout the day.
- Perform daily skin checks and use moisturizers as directed by a doctor to prevent breaks in the skin, which can lead to sores or infections.
- Elevate affected limbs while resting to help minimize swelling.
- Consider a reduced sodium diet to minimize swelling.
Experts also recommend avoiding excessive heat, such as prolonged periods in hot environments, soaking hot tubs, or applying hot compresses, as heat encourages additional swelling and may injure skin that is fragile from chronic edema.
Living with Truncal Lymphedema
While research on truncal lymphedema is still expanding, there are ample options for treatment to improve quality of life. It is possible to manage symptoms comfortably or prevent the development of lymphedema with the right interventions and lifestyle choices.
Many people are simply unaware of the signs and symptoms of truncal lymphedema. If you believe you are at risk for developing truncal lymphedema, or are experiencing any symptoms, discuss your questions and concerns with a physician.
Consider adding at-home compression therapy options to your lymphedema treatment plan, and discuss your home treatment options with your doctor. Lympha PressⓇ pneumatic compression therapy systems are backed by clinical studies showing more than 40 years of effectiveness in providing pain relief, reduction in swelling, and other positive results for people living with lymphedema.
For more information about treatment options for truncal lymphedema, please contact Lympha Press or take a look at our upper extremity garment options.
Share this post
Related Posts...
Explore
Contact Us.
We're ready to help.
Looking for more information, or to be connected with your local representative?
We can help. Fill out our contact form to get started.





