Dr. Jacalyn Brace, Ph.D. ANP-BC RN-BC WOCN
This is a 10-minute read.
Educating patients is one of my main missions and is critically important when it comes to lower extremity (LE) ulcers. Education helps us give ownership back to the patient and encourages them to make the best decisions possible for their long-term health outlook.
Proper diagnosis goes hand-in-hand with this mission. Various types of LE ulcers can seem the same at first glance, but can be quite different if you look more closely. When a patient arrives at my office, they usually have already seen a general practitioner, podiatrist, or another health provider. At this point, they are searching for a precise and accurate diagnosis.
In this article, we will explore the differential diagnosis of LE ulcers by examining underlying causes and various testing that I use to confirm the exact type of LE ulcer while also explaining the importance of addressing blood flow, pressure, and edema for proper healing.
Lower Extremity Ulcers and the Importance of Differential Diagnosis
LE ulcers develop from many etiologies, including arterial, venous, diabetes, and pressure. There is also some crossover among the types of ulcers.
A patient’s ulcer may be classified by some providers as an arterial or venous ulcer but ultimately the etiology of the ulcer is from pressure in addition to severe peripheral artery disease as discovered after a thorough assessment.
Differential diagnosis matters because the treatment for each depends heavily on the type of ulcer. For example, a “wet” ulcer should be treated quite differently from a “dry” ulcer, which we will explore in greater detail later in this article. For now, let’s take a closer look at how to identify each type of LE ulcer in a clinical setting.
Arterial Ulcers
An arterial ulcer is mainly found as a progressive occlusion that causes decreased blood flow. While the ulcer may be the result of trauma, we tend to look at more likely causes, such as stenosis and peripheral artery disease.
An examination should always start by cleaning the wound to provide a clear visual of the ulcer base and ensure that any cultures that are performed will not be contaminated. When examining the wound, if it is an arterial ulcer you will see that its edges normally have well-defined borders and the tissue is necrotic, dry, or very pale due to reduced blood flow. There is occasionally edema, but it remains very local to the ulcer.
Arterial ulcers most commonly occur below the ankle, often in the toes. In examining an arterial ulcer on the foot and toe, you would want to know the ABI, or ankle-brachial index. A normal ABI is 1.0 and an ABI of less than .8 would indicate the progression of the disease. The lower the ABI, the more significantly the disease has already progressed.
At this point, you would check the midfoot and toe pressure. In many cases, the ABI may be normal in the calf, but as you reach the toe it could be much worse. Does the patient have a reduced or absent pulse in the toe? The answer will help guide your next step.
In this case, I would recommend checking the area with Doppler or transcutaneous oxygen measurement (TCOM) if available during the patient’s office visit and ordering blood flow studies. The patient may need an arterial study to determine if there are clots and other disturbances in the blood flow.
Asking about the patient’s level of pain and type of pain are both recommended. Pain in the foot, especially at nighttime, is a red flag. With arterial ulcers, patients often describe a habit of dangling their feet in a chair or dangling their feet over the edge of the bed.
They’re exhibiting this behavior because when their feet are no longer dangling, they experience pain due to the lack of blood flow. Dangling the feet improves blood flow and relieves this pain.
Venous Ulcers
Compared to arterial ulcers, venous ulcers are usually larger in size and located closer to the ankle area, although this is just a guideline. Venous ulcers come in many sizes, shapes, and locations.
In a venous ulcer, the ulcer base is shallow in the beginning and the edges are quite irregular. These ulcers tend to have drainage from the wound, which is caused by edema. Edema causes the ulcers to generally have drainage, and the ulcer base can be pink, red, yellow, or brown/black if necrotic.
If the patient has venous stasis dermatitis, there will likely be more moisture to the skin surrounding the ulcer, even though the skin appears dry. When cleaning the patient’s leg, the dry skin sloughs off and is usually wet.
By the time the patient has been referred to me, these ulcers are often infected and have large amounts of drainage, because the patient has spent time treating themselves and/or waiting to see their general practitioner.
The key is to closely examine not just the tissue of the ulcer, but also the tissue around the ulcer. When blood seeps out of blood vessels, it can cause a stain. Peripheral vascular disease shows this characteristic staining, which becomes much worse as the disease progresses. This staining will not go away and once the stain is in place, it is there forever.
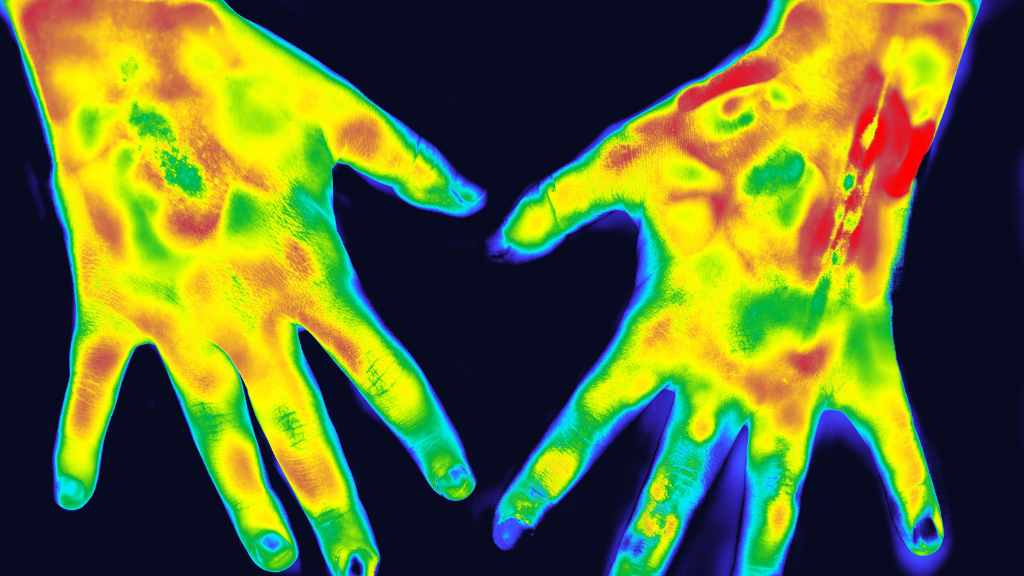
When examining a patient for edema, start at the front of the lower leg and work your way around to the ankle, examining the calf, knee, and thigh, assessing carefully all the way up the leg. Sometimes the foot is much worse than the calf. Edema may be compressing the arteries and decreasing this edema would improve blood flow throughout the leg.
Many venous ulcers tend to be infected and can’t be healed with a simple wrap and compression treatment. You wouldn’t wrap up this ulcer and say to the patient, “See you next week,” because this patient needs to be taught how to change the dressing daily and treat the infection.
Patients also need to understand the complexity of the ulcer. We’re not just treating the ulcer itself; we are also treating the surrounding skin. The surrounding skin may include dry, thick areas of tissue, as well as moist areas. This means we are dealing with a wet tissue, plus dry tissue treatment regimen. Wet skin needs absorption and dry skin needs hydration.
Pain during dangling occurs because of a buildup of venous congestion from venous insufficiency, which causes edema to increase. This means if the patient dangles their legs it will only become more painful. For these patients, elevation is what reduces the pain.
In terms of differential diagnosis of venous ulcers from arterial ulcers, it’s important to note that patients with venous ulcers complain of pain when the legs are dangling, unlike with arterial ulcers where dangling relieves the pain.
Diabetic Ulcers
Patients that have peripheral vascular disease or peripheral arterial disease may often be told they have an arterial or venous ulcer. However, it would be more accurate to say that they have a diabetic ulcer. You can help clear this up for your patient and educate them about the impact of diabetes.
Patients with diabetes have micro and macro vascular changes, peripheral neuropathy, and changes with the structure of their feet. This puts them at a higher risk for ulcer formation on their feet, which makes it harder for ulcers to heal.
Diabetic ulcers are normally present with a thick callus cliff appearance edge. The ulcer base is pink, red, yellow, or black. Infection can be present especially for patients who have uncontrolled diabetes.
Perhaps the person stepped on a piece of glass and a tiny shard became embedded in the foot. Maybe this person has thick, callused areas of the foot, which is common with diabetes. We should expect that it will be harder for this patient to heal than for someone without diabetes.
We should also check this patient’s shoes and see if they need diabetic shoes with inserts. They may need a forefoot offloading shoe, or another type of specialty shoe that addresses the forces happening between the footwear and the foot to enhance ulcer healing You must ensure that the person is educated about proper footwear that will prevent a recurrence of the diabetic ulcer.
Pressure Ulcers
Pressure ulcers form as a result of increased pressure to a certain location, usually the heel, ankle, forefoot, and toe. There are many risk factors for pressure ulcer development, but if pressure is the cause of the formation of the ulcer, we call it a pressure ulcer.
Let’s say a patient who has been diagnosed with peripheral arterial disease wears ill-fitting boots with a strap and then develops an ulcer from the strap. Although the patient has peripheral arterial disease, the pressure of the strap has caused the ulcer formation and the most accurate way to describe their ulcer is as a pressure ulcer.
With a pressure ulcer, it’s all about offloading the patient’s pressure sites. You must identify and eliminate the source of the pressure as you begin to address treating the ulcer. Patients need to float their heels off the bed with pillows placed under their calves from below the knee to the achilles. Additionally, patients need education on offloading techniques and devices.
Common Causes of Edema
Now, we will look at the causes of edema. Certain edema will usually go away on its own, like edema after an ankle or knee surgery, or even an open heart surgery. Maybe the person was in a motorcycle accident and had hip surgery.
In all of these situations, the patient might have edema after the surgery but with simple compression and a low-sodium diet, the edema will resolve on its own.
But what if you have a patient with a combination of factors? Perhaps this is someone with cardiac disease, renal disease, kidney disease, cancer, or an infection of the lymph nodes, but we don’t know that yet. In order to treat the edema, we will need to dig into the ultimate cause behind it.
I often see patients who have cancer and are receiving treatment with chemotherapy. Depending on the chemotherapy they’re receiving, and depending on their other health issues, they may get several liters of fluid as a part of their treatment.
For example, you may have a patient with cancer, cardiac disease, and renal disease receiving four liters of fluid to flush his kidneys. This patient is at the maximum amount of fluid he can take. His ulcer may look fine until he gets chemo, and then suddenly the ulcer appears worse again.
In this situation, you would need a cardiologist, oncologist, and all other doctors collaborating in harmony to serve this patient.
Infection can be another cause of edema. In this case, I look for unilateral signs, where one side of the body looks different than the other.
Why is their left leg swollen and their right leg isn’t? At this point, you may need to order a test to rule out a cause like lymphoma, and you may order blood flow studies to rule out a blood clot.
There are many reasons why patients may get blood clots in their legs. It could be a rare blood disorder, which can happen even in a very young patient. I have seen patients in their early 30s and 40s with a blood clot due to a blood disorder, a cardiac issue, or as a side effect of pregnancy and childbirth.
Edema is related to venous insufficiency, so you would need to order a study to see if there is normal compression and blood flow within the veins. If there are perforators or branches present within the blood vessel, this could cause problems in the lower extremities and the person could develop venous congestion with edema that includes blisters and ulcers.
Of course, the patient may describe it as starting with a simple bump, scratch, or itch. It’s common for a patient to relate a story of knocking their foot against a hard object, getting a cat scratch, or running their fingernails along a bug bite that turned into something much worse.
Or they may say they don’t remember a cause at all, but now the skin has begun to blister, peel, open up, and quite literally die.
Obesity can also be a contributor to edema. When someone is obese, it’s difficult for the blood to push through the body. If there is a significant pannus, there is pressure from the abdomen that prevents fluids in the groin from being able to move freely, and there is compression of the veins and arteries.
If we can support these patients to go into a weight loss program, cut down on fatty foods, and lose weight on their own, it may improve their overall health picture.
Better Treatment Through Early Diagnosis
To treat the underlying causes of ulcers, we must diagnose patients as early as possible and put a treatment plan together. This may involve a wide range of tests and studies.
PVR
This noninvasive vascular test is used to determine the arterial blood flow in the arms and legs.
Venous Reflux Ultrasound
This test visualizes the direction of blood flow and detects incompetent valves with veins, perforators, or branches of veins that may be present. Depending on where any abnormalities are found, intervention from a vein specialist may be needed.
Arterial Duplex Ultrasound
This test provides an interior view of the arteries to visualize any narrowing or blockages that may be present.
CTA Scan
This is a noninvasive test that uses a series of x-rays and scans to diagnose vascular pathologies.
X-rays
With all types of ulcers, some are deep enough that it could involve tendons and bones. In this case, we would do an X-ray to rule out infection of the bones.
At times, you may need an MRI for a more definitive diagnosis. You might need infectious disease, plastic surgery or podiatry involvement, plus medication to address the infection.
Albumin Levels
Although it’s easy to think of the albumin level as a diet marker, it can also signal inflammation and infection of the lower extremities. When someone has an infection, they could be losing albumin, or protein, through the drainage.
BNP
This indicates whether the patient has an exacerbation of congestive heart failure. The higher the number, the more severe the congestive heart failure.
CBC
The complete blood count looks at the platelets and whether you have low hemoglobin. It also looks at whether their white blood cells are elevated due to infection.
Chem 24
This is a complete profile and a complete blood panel test. It gives a more complete look at the person’s overall health picture.
Healing Ulcers
Finding the underlying cause of an ulcer is absolutely essential for proper treatment. Here’s a final example that illustrates why.
Perhaps a patient has an ulcer on their toe. After cleaning, examination, and testing, we see that the toe has dry gangrene and restricted blood flow. We learn that this patient has diabetes, and has been wearing work boots that put pressure on the toes. There are many issues we need to address here.
If you don’t treat the underlying issues, you won’t heal the ulcer. If we can keep this in mind while seeing our patients, we can help them receive the best care possible while staying educated and vigilant about their health situation.
About the Author
Dr. Jacalyn Brace is a Certified Adult Nurse Practitioner and holds a Ph.D. from The University of Virginia. She is affiliated with the Cleveland Clinic Heart & Vascular Institute and is a well-known speaker on the topics of NPWT, ulcers, edema, and vascular disease.
About this Series
This story series is a partnership of Lympha Press and Medical Solutions Supplier. For 25 years, Medical Solutions Supplier has provided innovative compression pump home therapy equipment that supports the best possible patient outcomes.